Transcutaneous Electrical Nerve Stimulation – TENS
Author: Vladimir Kaye, MD, Consulting Staff, Departments of Neurology and Psychiatry, Hoag Hospital Coauthor(s): Murray E Brandstater, MBBS, PhD, Chairman and Program Director, Professor, Department of Physical Medicine and Rehabilitation, Loma Linda University School of Medicine Contributor Information and Disclosures
Updated: Oct 8, 2008
Introduction to TENS
Transcutaneous electrical nerve stimulation (TENS) currently is one of the most commonly used forms of electroanalgesia. Hundreds of clinical reports exist concerning the use of TENS for various types of conditions, such as low back pain (LBP), myofascial and arthritic pain, sympathetically mediated pain, bladder incontinence, neurogenic pain, visceral pain, and postsurgical pain. Because many of these studies were uncontrolled, there has been ongoing debate about the degree to which TENS is more effective than placebo in reducing pain.
The currently proposed mechanisms by which TENS produces neuromodulation include the following:
Presynaptic inhibition in the dorsal horn of the spinal cord
Endogenous pain control (via endorphins, enkephalins, and dynorphins)
Direct inhibition of an abnormally excited nerve
Restoration of afferent input
The results of laboratory studies suggest that electrical stimulation delivered by a TENS unit reduces pain through nociceptive inhibition at the presynaptic level in the dorsal horn, thus limiting its central transmission. The electrical stimuli on the skin preferentially activate low-threshold, myelinated nerve fibers. The afferent input from these fibers inhibits propagation of nociception carried in the small, unmyelinated C fibers by blocking transmission along these fibers to the target or T cells located in the substantia gelatinosa (laminae 2 and 3) of the dorsal horn.
Studies show marked increases in beta endorphin and met-enkephalin with low-frequency TENS, with demonstrated reversal of the antinociceptive effects by naloxone. These effects have been postulated to be mediated through micro-opioid receptors. Research indicates, however, that high-frequency TENS analgesia is not reversed by naloxone, implicating a naloxone-resistant, dynorphin-binding receptor. A sample of cerebral spinal fluid in those subjects demonstrated increased levels of dynorphin A.
The mechanism of the analgesia produced by TENS is explained by the gate-control theory proposed by Melzack and Wall in 1965.7 The gate usually is closed, inhibiting constant nociceptive transmission via C fibers from the periphery to the T cell. When painful peripheral stimulation occurs, however, the information carried by C fibers reaches the T cells and opens the gate, allowing pain transmission centrally to the thalamus and cortex, where it is interpreted as pain. The gate-control theory postulates a mechanism by which the gate is closed again, preventing further central transmission of the nociceptive information to the cortex. The proposed mechanism for closing the gate is inhibition of the C-fiber nociception by impulses in activated myelinated fibers.
Technical Considerations of Transcutaneous Electrical Nerve Stimulation
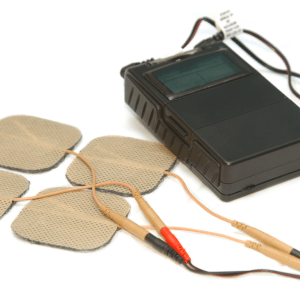
A transcutaneous electrical nerve stimulation (TENS) unit consists of 1 or more electrical-signal generators, a battery, and a set of electrodes. The TENS unit is small and programmable, and the generators can deliver trains of stimuli with variable current strengths, pulse rates, and pulse widths. The preferred waveform is biphasic, to avoid the electrolytic and iontophoretic effects of a unidirectional current. The usual settings for the stimulus parameters used clinically are the following:
Amplitude – Current at a comfortable, low intensity level, just above threshold
Pulse width (duration) – 10-1000 microseconds
Pulse rate (frequency) – 80-100 impulses per second (Hz); 0.5-10 Hz when the stimulus intensity is set high
When Transcutaneous Electrical Nerve Stimulation is used analgesically, patients are instructed to try different frequencies and intensities to find those that provide them with the best pain control. Optimal settings of stimulus parameters are subjective and are determined by trial and error. Electrode positioning is quite important. Usually, the electrodes are initially placed on the skin over the painful area, but other locations (eg, over cutaneous nerves, trigger points, acupuncture sites) may give comparable or even better pain relief.
The 3 options for the standard settings used in different therapeutic methods of TENS application include the following:
Conventional TENS has a high stimulation frequency (40-150 Hz) and low intensity, just above threshold, with the current set between 10-30 mA. The pulse duration is short (up to 50 microseconds). The onset of analgesia with this set up is virtually immediate. Pain relief lasts while the stimulus is turned on, but it usually abates when the stimulation stops. Patients customarily apply the electrodes and leave them in place all day, turning the stimulus on for approximately 30-minute intervals throughout the day. In individuals who respond well, analgesia persists for a variable time after the stimulation stops.
In acupuncture like settings, the TENS unit delivers low frequency stimulus trains at 1-10 Hz, at a high stimulus intensity, close to the tolerance limit of the patient. Although this method sometimes may be more effective than conventional TENS, it is uncomfortable, and not many patients can tolerate it. This method often is considered for patients who do not respond to conventional TENS.
Pulsed (burst) TENS uses low-intensity stimuli firing in high-frequency bursts. The recurrent bursts discharge at 1-2 Hz, and the frequency of impulses within each burst is at 100 Hz. No particular advantage has been established for the pulsed method over the conventional TENS method.
Patient comfort is a very important determinant of compliance and, consequently, of the overall success of treatment. The intensity of the impulse is a function of pulse duration and amplitude. Greater pulse widths tend to be more painful. The acupuncture like method is less tolerable, because the impulse intensity is higher.
The amount of output current depends on the combined impedance of the electrodes, skin, and tissues. With repetitive electrical stimuli applied to the same location on the skin, the skin impedance is reduced, which could result in greater current flow as stimulation continues. A constant current stimulator, therefore, is preferred in order to minimize sudden, uncontrolled fluctuations of current intensity related to changes in impedance. An electro conductive gel applied between the electrode and skin serves to minimize the skin impedance.
Medical complications arising from use of Transcutaneous Electrical Nerve Stimulation are rare. However, skin irritation can occur in as many as 33% of patients, due, at least in part, to drying out of the electrode gel. Patients need to be instructed in the use and care of TENS equipment, with particular attention to the electrodes.
In some cases, individuals react to the tape used to secure the electrodes. Skin irritation is minimized by using disposable, self-adhesive electrodes and repositioning them slightly for repeated applications. The use of TENS is contraindicated in patients with a demand-type pacemaker, because the stimulus output of the TENS unit may drive or inhibit the pacemaker.
Newer TENS Modalities
A variety of newer transcutaneous or percutaneous electrical stimulation modalities have emerged. They include the following:
Interferential current therapy (IFC) is based on summation of 2 alternating current signals of slightly different frequency. The resultant current consists of a cyclical modulation of amplitude, based on the difference in frequency between the 2 signals. When the signals are in phase, they summate to an amplitude sufficient to stimulate, but no stimulation occurs when they are out of phase. The beat frequency of IFC is equal to the difference in the frequencies of the 2 signals. For example, the beat frequency and, hence, the stimulation rate of a dual channel IFC unit with signals set at 4200 and 4100 Hz is 100 Hz.
IFC therapy can deliver higher currents than TENS can. IFC can use 2, 4, or 6 applicators, arranged in either the same plane, for use on such regions as the back, or in different planes in complex regions (eg, the shoulder).
Percutaneous electrical nerve stimulation (PENS) combines advantages of electro acupuncture and TENS. Rather than using surface electrodes, PENS uses acupuncture like needle probes as electrodes, with these placed at dermatomal levels corresponding to local pathology. The main advantage of PENS over TENS is that it bypasses local skin resistance and delivers electrical stimuli at the precisely desired level in close proximity to the nerve endings located in soft tissue, muscle, or periosteum.3
Applications of Tens in Clinical Practice
 Literature on the effectiveness of transcutaneous electrical nerve stimulation (TENS) in a variety of medical conditions reports a wide range of outcomes, from very positive to negative. Currently, there is an overall consensus favoring the use of TENS, with authorities differing on its value in different clinical situations. Generally, TENS provides initial relief of pain in 70-80% of patients, but the success rate decreases after a few months or longer to around 20-30%. To exclude a false-negative response, a trial of TENS for at least 1 hour should be given to confirm potential benefit from subsequent continuous use.
Literature on the effectiveness of transcutaneous electrical nerve stimulation (TENS) in a variety of medical conditions reports a wide range of outcomes, from very positive to negative. Currently, there is an overall consensus favoring the use of TENS, with authorities differing on its value in different clinical situations. Generally, TENS provides initial relief of pain in 70-80% of patients, but the success rate decreases after a few months or longer to around 20-30%. To exclude a false-negative response, a trial of TENS for at least 1 hour should be given to confirm potential benefit from subsequent continuous use.
According to Johnson, the time from the start of stimulation to the onset of analgesia varies from almost immediate to hours (on average, 20-30 minutes in over 75% of patients and 1 hour in 95% of patients).8 The duration of analgesia also varies considerably, continuing only for the duration of stimulation in some patients and providing considerable, prolonged post stimulation relief in others. The same TENS protocol may have different degrees of anti nociception in acute experimental pain compared with chronic clinical pain in patients with chronic low back pain (LBP).9
Patients differ in their stimulus preferences and in their rates of compliance. In Johnson’s study of compliance in patients who benefited from TENS, 75% used the device on a daily basis. Patients showed individual preferences for particular pulse frequencies and patterns, and they consistently adjusted their stimulators to these settings in subsequent treatment sessions.
Indications for the use of TENS
1. Neurogenic pain (eg, deafferentation pain, phantom pain), sympathetically mediated pain, postherpetic neuralgia, trigeminal neuralgia, atypical facial pain, brachial plexus avulsion, pain after spinal cord injury (SCI)
2. Musculoskeletal pain – Examples of specific diagnoses include joint pain from rheumatoid arthritis and osteoarthritis, acute postoperative pain (eg, postthoracotomy), and acute posttraumatic pain.10, 11, 12, 13, 14, 15, 16 After surgery, TENS is most effective for mild to moderate levels of pain, and it is ineffective for severe pain. The use of TENS in chronic LBP and myofascial pain is controversial, with placebo-controlled studies failing to show statistically significant beneficial results. Uncertainty also exists about the value of TENS in tension headache.
3. Visceral pain and dysmenorrhea – TENS has been successfully applied to these conditions as well.17
4. Other disorders – TENS has been used successfully in patients with angina pectoris and urge incontinence, as well as in patients requiring dental anesthesia.18, 19 Reports discuss the use of TENS to assist patients in regaining motor function following stroke, to control nausea in patients undergoing chemotherapy, as an opioid -sparing modality in postoperative recovery, and in postfracture pain.20, 21, 22, 23, 24, 25, 26
Contraindications for the use of TENS
TENS should not be used in patients with a pacemaker (especially of the demand type).
TENS should not be used during pregnancy, because it may induce premature labor.
TENS should not be applied over the carotid sinuses due to the risk of acute hypotension through a vasovagal reflex.
TENS should not be placed over the anterior neck, because laryngospasm due to laryngeal muscle contraction may occur.
The electrodes should not be placed in an area of sensory impairment (eg, in cases of nerve lesions, neuropathies), where the possibility of burns exists.
A TENS unit should be used cautiously in patients with a spinal cord stimulator or an intrathecal pump.
Comparison Between Tens and Other Electrical Modalities
A number of studies have compared transcutaneous electrical nerve stimulation (TENS) with similar therapeutic modalities, including percutaneous electrical nerve stimulation (PENS), interferential current therapy (IFC), and acupuncture.17, 27 The results included the following:
- In one study of elderly patients with chronic low back pain (LBP), acupuncture and TENS had demonstrable benefits, with the acupuncture group demonstrating improvement in spinal flexion.
- In patients with chronic LBP and sciatica, PENS was more effective than TENS in providing short-term pain relief and improved function, including an improved quality of sleep and sense of well-being.
- Overall, 91% and 73% of patients, respectively, chose PENS as the preferred modality for pain relief in LBP and sciatica.
PENS has been used successfully for pain relief in patients with acute herpes zoster and in persons suffering from cancer with bony metastases. - IFC and TENS had a statistically significant effect on the median nerve excitation threshold in young women.
Transcutaneous Electrical Nerve Stimulation for Pain
Using Elecitrical Stimulation for Pain is not new concept. Several modalities of electrical stimulation exist for the treatment of chronic pain. Below are some examples and explanations:
TENS:
Transcutaneous Electrical Nerve stimulator is a device used to treat chronic intractable pain, and pain associated with active or post- traumatic injury unresponsive to other standard pain therapies. The device is applied to the surface of the skin at the site of the pain. It consists of an electrical pulse generator, usually battery operated, connected by a wire to two or more electrodes. A programmable stimulator may be programmed in advance to stimulate at regular times or upon demand by the use of a hand held magnet over the stimulator. ( Neuro Cybernetic Prosthesis System )
MNS:
Microcurrent Nerve Stimulator works on the same principal as TENS by delivering microcurrent instead of regular current.
PENS:
Percutaneous Nerve Stimulator is similar to TENS, with the exception that instead of electrodes attached to the skin near the pain area, in PENS, a needle is inserted into the pain site.
PNT:
Percutaneous neuromodulation therapy is a variant of PENS in which up to 10 fine filament electrodes are temporarily placed at specific anatomical landmarks in the back. Treatment regimens consist of 30-minute sessions, once or twice a week for 8 to 10 sessions.
VNS:
Vagus Nerve Stimulation Implanted vagus nerve stimulation (VNS) devices have been used to treat patients with medically refractory partial-onset seizures for whom surgery is not recommended or for whom surgery has failed. Surgery for implantation of the VNS device is done with the patient under either general anesthesia or regional cervical block. Since right vagus nerve stimulation produces bradycardia, implantation is limited to left-sided unilateral implantations. Two spiral electrodes are implanted around the left vagus nerve within the carotid sheath, which are connected to an infraclavicular generator pack. A programmable stimulator may be programmed in advance to stimulate at regular times or upon demand by the use of a hand held magnet over the stimulator. ( Neuro Cybernetic Prosthesis System )
FNS
Functional Neuromuscular Stimulation attempts to replace stimuli from destroyed nerve pathways with electrical stimulation to the muscles. It is presumed that electric stimulation enables the spinal cord injured patient to stand or walk independently, or to maintain healthy muscle tone and strength.
NMES
Neuromuscular Electric Stimulator for disuse atrophy. NMES involves the use of a device that transmits an electrical impulse to activate muscle groups by way of electrodes. There are two broad categories of NMES. One type of device stimulates the muscle when the patient is in a resting state to treat muscle atrophy. The second type is used to enhance functional activity of neurologically impaired patients.
Spinal Cord Stimulation for Chronic Pain:
Electrodes are implanted in the epidural space to stimulate the dorsal column and treat chronic pain. Learn more about when they use spinal cord stimulators.
DBS
Deep Brain Stimulation of the thalamus has been used as an alternative to permanent neuroablative procedures such as thalamotomy and pallidotomy for control of essential tremor, and tremors associated with Parkinson’s disease. It involves stereotactic placement of an electrode into the brain, which is attached to a temporary transcutaneous cable for short-term stimulation to validate treatment effectiveness. Several days later a permanent subcutaneous programmable stimulator is implanted. DBS of the globus pallidus and subthalamic nucleus has also been investigated for other symptoms of Parkinson’s disease such as rigidity, bradykinesia or akinesia. DBS is also FDA approved for the treatment of dystonia.
H-Wave ® Electric Stimulation
This device is used for the treatment of pain related to a variety of etiologies. This is also used for wound healing.
Sensory Stimulation for Coma Patients
Sensory stimulation is intended to enhance awakening and rehabilitative potential of coma patients. Treatment may be delivered in the hospital, the patient’s home, or a nursing home by professionals including nurses, occupational therapist, physical therapist, speech language therapist and even by a trained family member.
TES
Threshold Electric Stimulator as a treatment of motor disorders. Low intensity electrical stimulation is used to target spastic muscles during sleep at home. Although the exact mechanism of action is not known, it is presumed that it may increase muscle strength and joint mobility leading to improved voluntary motor function. This is used in children with spastic paraplegia related to cerebral palsy and also in those with other motor disorders, such as spina bifida.
Sympathetic therapy as a treatment of chronic pain (i.e. Dynatron STS)
Sympathetic therapy describes a type of electrical stimulation of the peripheral nerves that is designed to stimulate the sympathetic nervous system in an effort to ‘normalize’ the autonomic nervous system and alleviate chronic pain. Sympathetic therapy is not designed to treat local pain, but is designed to induce a systemic effect on sympathetically induced pain.
Interferential current stimulation (IFC)
IFC is a type of electrical current treatment that uses paired electrodes of two independent medium-frequency alternating currents. The electrodes are arranged on the skin so the current flowing between each pair intersects at the underlying target. IFC has been investigated as a technique to reduce pain, improve range of motion, or promote local healing.
Lymphavision TM
This is an electrical stimulation device that stimulates smooth muscles thereby promoting lymphatic flow. It is described as a treatment for such conditions as diabetic foot syndrome and trophic ulcers, and prevention of deep vein thrombosis.
TEJS
Transcutaneous electrical joint stimulation is the application of a signal-specific electrical current to the joint tissue to relive the signs and symptoms of osteoarthritis of the knee. Two electrode patches are worn for six to ten hours a day, preferably while the patient is sleeping. TEJS has been indicated as adjunctive therapy for patients who have failed NSAIDS, those with moderate to severe disease despite best medical therapy, and those with severe disease who are not surgical candidates for reasons such as morbid obesity and inappropriate age.
PES
Pulsed electrical stimulation is provided by an electronic device that noninvasively delivers a low voltage, monophasic electrical field to the targeted area of pain. It is used to improve functional status and relieve pain related to osteoarthritis and rheumatoid arthritis unresponsive to other standard forms of treatment.
Reference: Wellmark, Blue Cross Blue Shield.